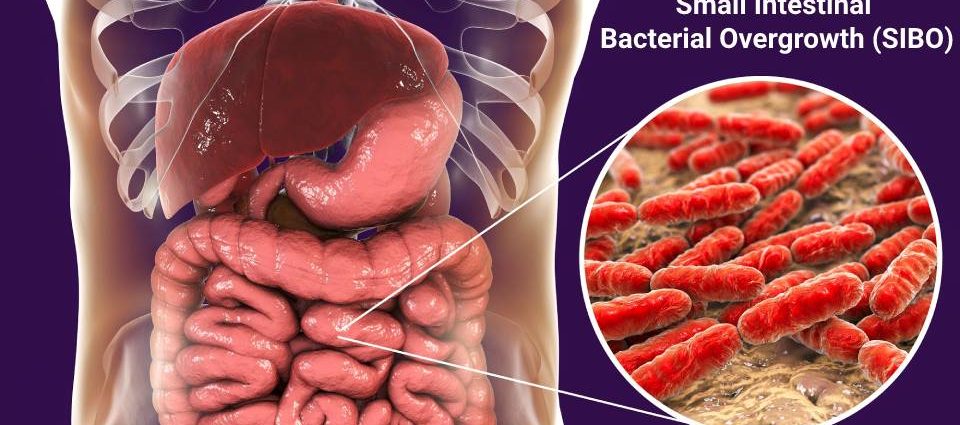
Small Intestinal Bacterial Overgrowth (SIBO) occurs when there is an abnormal increase in the number of bacteria in the small intestine. Typically, the small intestine contains relatively low numbers of bacteria, unlike the colon, which is densely populated. When the balance of bacteria in the small intestine is disrupted, it can lead to a variety of symptoms and health issues. SIBO is often misunderstood and can be misdiagnosed due to the overlap of its symptoms with other gastrointestinal disorders.
Understanding SIBO is essential for addressing gut health issues effectively. This condition can impact nutrient absorption, lead to inflammation, and cause various digestive symptoms. It’s important to recognize the signs of SIBO and understand its causes to seek proper treatment and management. In the following sections, we will dive deeper into the symptoms, causes, and treatment options for SIBO, shedding light on how to improve gut health and overall well-being.
Symptoms of SIBO
Image courtesy: Unsplash
Small Intestinal Bacterial Overgrowth (SIBO) is a condition that, though often overlooked, can significantly disrupt an individual’s life. Recognizing the symptoms early can lead to quicker diagnosis and treatment, improving quality of life.
Common symptoms to look out for
The symptoms of SIBO can vary widely from person to person, but some are more common than others. These include:
- Abdominal discomfort and bloating: One of the hallmark symptoms of SIBO is a feeling of bloating and discomfort in the abdominal area. This symptom can be exacerbated after eating and may come and go in intensity.Excessive gas and belching: An increase in bacterial fermentation within the small intestine often leads to excess gas production, resulting in an uncomfortable amount of flatulence and belching.
– Diarrhea, constipation, or a mix of both: Individuals with SIBO may experience alterations in bowel habits, including diarrhea, constipation, or a combination of both. The changes in bowel movements are due to the imbalance of bacteria affecting the natural digestive processes.
– Nausea and loss of appetite: As the digestive tract is directly impacted by SIBO, symptoms can include nausea and a general decrease in appetite. In some cases, this can lead to unintended weight loss.
– Nutrient deficiencies: Over time, SIBO can lead to difficulties in nutrient absorption, resulting in deficiencies. Common deficiencies include vitamins B12 and D, iron, and fat-soluble vitamins, which may lead to symptoms like anemia, fatigue, and bone pain.
– General fatigue and weakness: The impact of SIBO on nutrient absorption can lead to a general feeling of tiredness and weakness, often due to the body’s inability to get the necessary energy and nutrients from the food consumed.
Recognizing these symptoms is crucial for seeking appropriate treatment. If you are experiencing a combination of these symptoms, it is essential to consult with a healthcare provider for further investigation and to rule out other possible conditions.
Causes of SIBO:
Understanding the causes of SIBO is key to prevention and effective treatment. While the exact cause of SIBO can vary from one individual to another, several factors have been identified that contribute to the development of this condition.
Factors That Contribute to SIBO Development:
Several elements can predispose an individual to developing SIBO. These factors disrupt the normal ecosystem of the gut, allowing for an overgrowth of bacteria in the small intestine:
- Altered gut motility: Reduced motility in the small intestine can prevent the normal clearing of bacteria, leading to its overgrowth. Conditions such as diabetes, scleroderma, or post-surgical changes can contribute to this altered motility.
- Anatomic abnormalities of the small intestine: Structural problems, such as diverticula, fistulas, or strictures, can create pockets where bacteria can grow excessively.
- Gastric acid suppression: The use of proton pump inhibitors (PPIs) reduces stomach acid, which can increase susceptibility to bacterial overgrowth. Stomach acid plays a crucial role in controlling the bacterial population entering the small intestine from the mouth.
- Impaired immune function: An immune system that is compromised, either due to medical treatment like chemotherapy or diseases such as HIV/AIDS, may not be able to regulate the bacterial population effectively.
- Dietary factors: A diet high in sugars and carbohydrates may promote the growth of bacteria in the small intestine, exacerbating the condition.
- Use of certain medications: Besides PPIs, other medications like narcotics (which can decrease gut motility) and antibiotics (which can disrupt the normal gut flora) might contribute to the development of SIBO.
Understanding these contributing factors is essential in managing and preventing SIBO. Modification of risk factors, where possible, combined with appropriate medical treatment, can help mitigate the symptoms and long-term impacts of SIBO. When dealing with gastrointestinal symptoms that persist, seeking medical advice is crucial to obtaining a correct diagnosis and appropriate treatment plan.
Diagnosis of SIBO:
Understanding the nuances involved in diagnosing Small Intestinal Bacterial Overgrowth (SIBO) is crucial for both patients and healthcare professionals. Achieving an accurate diagnosis involves a combination of methods, each playing a pivotal role in identifying this condition, which often masquerades as other digestive disorders.
Methods Used to Diagnose SIBO:
The diagnosis of SIBO is anchored on a few key methods that provide insight into the bacterial environment within the small intestine.
- Breath Tests: The most common non-invasive test for diagnosing SIBO involves measuring hydrogen and methane levels in the breath after the patient ingests a sugar solution. Elevated levels of these gases can indicate bacterial overgrowth, as they are byproducts of bacterial metabolism.
- Small Intestinal Aspirate and Fluid Culture: Considered the gold standard, this procedure involves taking a sample from the small intestine and culturing it to identify bacterial growth. It is more invasive than breath tests and is typically used when other tests are inconclusive.
- Blood Tests: While not directly diagnosing SIBO, blood tests can identify complications or indications of SIBO, such as vitamin deficiencies or elevated levels of certain markers that suggest inflammation.
- Stool Tests: These are generally used to rule out other conditions, as they cannot accurately diagnose SIBO. However, stool tests can provide valuable information about the overall health of the digestive system.
Importance of Seeking Medical Advice for Diagnosis:
Self-diagnosis and treatment of suspected SIBO can lead to a worsening of symptoms or masking of other serious digestive disorders. It’s paramount for individuals who suspect they have SIBO to consult with healthcare professionals. Gastroenterologists and specialized dietitians can offer comprehensive testing and diagnosis, ensuring that the treatment plan is tailored to the specific needs and severity of the condition in each patient.
Treatment Options for SIBO:
Once diagnosed, the treatment for SIBO typically involves a multi-faceted approach, integrating dietary modifications, medication, and lifestyle adjustments to manage and mitigate symptoms and underlying causes.
Dietary Changes and Restrictions:
Diet plays a significant role in managing SIBO, as certain foods can exacerbate bacterial overgrowth and symptoms. Common dietary recommendations include:
- Low-FODMAP Diet: Reducing the intake of foods high in Fermentable Oligo-, Di-, Mono-saccharides, And Polyols (FODMAPs) can help minimize the symptoms of SIBO, as these are types of carbohydrates that can ferment in the gut, feeding bacterial overgrowth.
- Gluten-Free Diet: For some individuals, eliminating gluten can alleviate symptoms, especially if there is an underlying sensitivity or celiac disease.
- Specific Carbohydrate Diet (SCD): This diet excludes many types of carbohydrates, including grains and sugar, to reduce bacterial fermentation.
It’s essential to navigate these dietary changes under the guidance of a healthcare professional to ensure nutritional needs are met and to avoid unnecessary restrictions.
Medications Commonly Prescribed for SIBO:
Treatment often includes medications to reduce bacterial overgrowth and alleviate symptoms:
- Antibiotics: Typically, a key component of treatment, antibiotics like rifaximin, are used to decrease bacterial numbers in the small intestine.
- Prokinetics: These drugs can help increase the movement of the small intestine, preventing the stasis of food and bacteria that can lead to or worsen SIBO.
- Probiotics and Prebiotics: While their role is still under research, probiotics and prebiotics can sometimes be recommended to help balance the gut microbiome.
Lifestyle Adjustments to Manage SIBO Symptoms:
In addition to dietary changes and medication, incorporating lifestyle adjustments can be beneficial in managing SIBO:
- Regular Exercise: Promotes gut motility and can help alleviate symptoms.
- Stress Management: Stress can exacerbate symptoms of SIBO. Practices such as meditation, yoga, and mindful breathing can help manage stress levels.
- Sleep Hygiene: Ensuring adequate sleep can support the body’s overall health, including the digestive system.
By combining these treatment strategies, individuals with SIBO can often see significant improvements in their symptoms and overall quality of life. However, due to the complex nature of SIBO, ongoing monitoring and adjustments to the treatment plan may be necessary, under the guidance of healthcare professionals.
Prognosis and long-term management of SIBO:
Managing Small Intestinal Bacterial Overgrowth (SIBO) requires a comprehensive approach to ensure long-term relief and prevent recurrences. With appropriate treatment and lifestyle adjustments, the prognosis for SIBO is generally positive. Most individuals experience significant improvement in their symptoms. However, since SIBO can recur, ongoing management may be necessary.
- Dietary Modifications: Maintaining a diet that limits foods that ferment in the gut is crucial. This includes reducing the intake of certain carbohydrates and sugars that feed the excessive bacteria in the small intestine. A registered dietitian can provide personalized dietary advice.
- Medication and Antibiotics: In some cases, a course of antibiotics is prescribed to reduce bacterial overgrowth. Following this, medications to promote gut motility or supplements to improve digestive function may be recommended.
- Routine Monitoring: Regular follow-ups with a healthcare provider to monitor symptoms and potentially adjust treatment plans are important. This may include repeat testing to check the effectiveness of treatments.
- Lifestyle Changes: Incorporating exercise, stress reduction techniques, and ensuring adequate hydration can support gut health and reduce the risk of SIBO recurrence.
Managing SIBO effectively involves a partnership between the patient and the healthcare team, focusing on both treatment and prevention strategies. Changes in symptoms should be communicated promptly, as early intervention can help in adjusting the management plan for better outcomes.