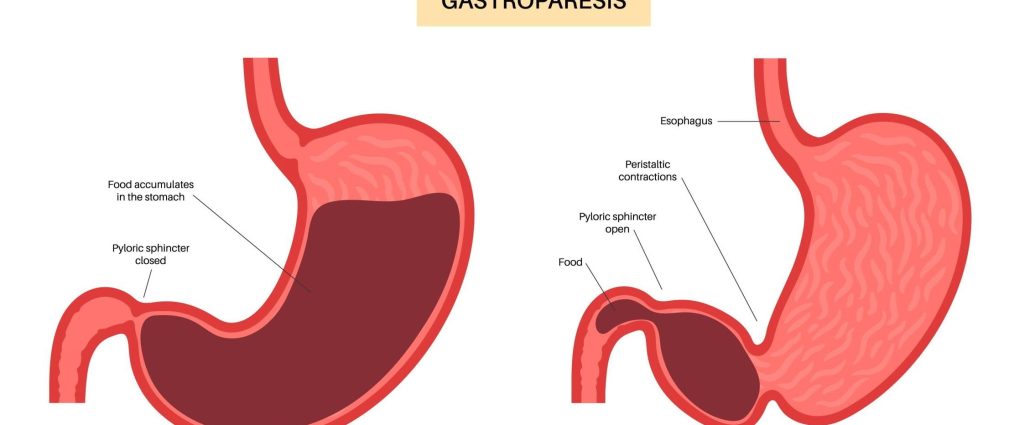
Gastroparesis is a chronic condition that affects the normal spontaneous movement of the muscles (motility) in your stomach. Normally, strong muscular contractions propel food through your digestive tract. But in gastroparesis, your stomach’s motility works poorly or not at all, preventing your stomach from emptying properly. This delay can lead to a variety of symptoms and complications that affect digestion and overall quality of life.
Understanding gastroparesis is crucial for managing its symptoms and seeking appropriate treatment. This condition underscores the importance of digestive health and the complex mechanisms behind the body’s ability to process and absorb nutrients from the food we consume.
Gastroparesis: Overview of Common Symptoms
Gastroparesis, a condition characterized by delayed gastric emptying, manifests through various symptoms that can significantly affect an individual’s quality of life. The most common symptom is a feeling of fullness after eating only a small amount of food. This sensation, also known as early satiety, can lead to inadequate nutritional intake if not addressed. Nausea is another frequent complaint among those with gastroparesis, often accompanied by vomiting, particularly of undigested food that has remained in the stomach for hours after eating.
Abdominal bloating and pain are also typical, resulting from the abnormal retention and fermentation of food in the stomach. Gastroesophageal reflux, more commonly referred to as heartburn or acid reflux, occurs when stomach contents flow back into the esophagus, causing discomfort and potential damage to the esophageal lining. Lastly, fluctuations in blood glucose levels can be a consequence of erratic food digestion, posing additional challenges for individuals, especially those with diabetes.
Impact on daily life
The impacts of gastroparesis symptoms on daily life extend beyond physical discomfort and nutritional challenges. The unpredictability of symptoms can lead to anxiety around meal times and social gatherings, where food plays a central role. Individuals may experience a decreased appetite due to fear of ensuing pain or discomfort, leading to unintentional weight loss and malnutrition.
Furthermore, recurring nausea and vomiting can impede one’s ability to maintain a regular work or school schedule, contributing to stress and isolation. The constant management required to mitigate symptoms, including dietary changes, medication schedules, and medical appointments, often requires significant time and effort, heightening the emotional and psychological toll of the condition.
Causes of Gastroparesis:
- Underlying Medical Conditions
Several underlying medical conditions have been identified as potential causes of gastroparesis, demonstrating the complexity of this disorder. Diabetes mellitus is among the most common, with high blood glucose levels over time leading to damage of the vagus nerve, responsible for controlling stomach muscle contractions. This impairment hinders the stomach’s ability to empty efficiently. Another contributor can be surgeries that involve the stomach or vagus nerve, which may inadvertently affect stomach motility.
Neurological conditions such as Parkinson’s disease and multiple sclerosis can also lead to gastroparesis by affecting the nerves that manage stomach contractions. Less commonly, connective tissue diseases such as scleroderma can impact the stomach lining and muscles, further complicating gastric emptying processes. Additionally, infections, particularly viral ones, have been noted to trigger gastroparesis in some cases, though these instances are typically temporary.
- Risk Factors
Apart from underlying medical conditions, certain risk factors have been identified in association with gastroparesis. Gender plays a notable role, with women diagnosed more frequently than men. This discrepancy may be attributed to differences in stomach motility or hormonal influences, though the exact reasons remain under study. Medications that slow gastric emptying, such as narcotics and some antidepressants, can also raise the risk of developing gastroparesis, emphasizing the importance of medication review and management.
Lifestyle factors, including diet and smoking, have been linked to stomach motility disorders, suggesting that healthful living practices may play a role in prevention and management. Understanding these risk factors is crucial for both individuals and healthcare providers in identifying and addressing potential cases of gastroparesis effectively.
Diagnosis and Testing for Gastroparesis:
Diagnosing gastroparesis involves several steps to accurately determine the presence and severity of the disorder. It is essential to distinguish this condition from others with similar symptoms such as acid reflux or irritable bowel syndrome.
Common Diagnostic Methods
The primary methods for diagnosing gastroparesis include:
- Gastric emptying study: This is the most crucial test for diagnosing gastroparesis, during which the patient eats a meal containing a small amount of radioactive material. Then, a scanner tracks the rate at which the stomach empties the meal into the small intestine. A delay in this process indicates gastroparesis.
- Endoscopy: To rule out other conditions that might be causing the symptoms, an endoscopy might be performed. During this procedure, a thin tube with a camera is passed down the throat into the stomach to visualize the upper digestive tract.
- Ultrasound: This imaging test examines the organs in the abdomen, looking for abnormalities that might contribute to gastroparesis symptoms, such as gallstones.
- Blood tests: Basic blood tests might be conducted to check for signs of infection, electrolyte imbalances, or glucose levels that could be influencing the symptoms.
Importance of Early Detection
Early detection of gastroparesis is crucial for several reasons:
- Prevent complications: By identifying gastroparesis early, it’s possible to take steps to prevent complications such as severe dehydration, malnutrition, and the formation of bezoars (solid masses of food).
- Enhance quality of life: Early intervention can significantly improve a patient’s quality of life by managing symptoms such as nausea, vomiting, and abdominal pain more effectively.
- Customize treatment plans: Identifying the condition early allows healthcare providers to tailor treatment plans to individual needs, potentially preventing the condition from worsening.
Treatment Options for Gastroparesis:
The treatment of gastroparesis focuses on managing symptoms and facilitating gastric emptying. Since there is no cure for the disorder, treatment aims to improve the patient’s quality of life and nutritional status.
Dietary Changes and Meal Planning
Dietary modification is a cornerstone in managing gastroparesis. Key recommendations include:
- Eating smaller, more frequent meals: This approach can help manage symptoms by reducing the workload on the stomach at any given time.
- Choosing low-fiber and low-fat foods: High-fiber and high-fat foods can slow down gastric emptying. Patients are advised to opt for easily digestible foods to ease stomach processing.
- Staying hydrated: Drinking enough fluids is essential, especially for those who frequently vomit due to gastroparesis.
Medications for Symptom Management
Medications play a critical role in symptom management for gastroparesis sufferers:
- Prokinetic agents: These medications help speed up the movement of contents through the stomach.
- Anti-nausea drugs: Drugs to control nausea and vomiting are often prescribed to improve the patient’s comfort and prevent dehydration.
Surgical Interventions
In severe cases of gastroparesis, where dietary changes and medications do not bring relief, surgical options may be considered:
- Gastric electrical stimulation: A device is implanted to send mild electrical pulses to the stomach’s muscles, encouraging motility.
- Jejunostomy: A feeding tube may be placed directly into the small intestine in extreme cases, bypassing the stomach altogether to ensure nutrition can be maintained.
Each treatment plan is highly individualized, emphasizing the importance of a comprehensive diagnostic evaluation to guide therapeutic decisions. Through proper management, many patients can achieve significant symptom relief and improved quality of life.
Lifestyle Tips for Managing Gastroparesis:
Living with gastroparesis can require adjustments in various aspects of lifestyle to manage symptoms effectively. Besides medical treatment, certain lifestyle changes can help in alleviating symptoms and improving quality of life.
Stress Management Techniques
Stress can exacerbate the symptoms of gastroparesis, leading to a cycle of discomfort and anxiety. Stress management is a crucial aspect of managing this condition. Techniques such as deep-breathing exercises, meditation, and yoga can significantly reduce stress levels. Additionally, finding hobbies that relax the mind and body can also be beneficial. It’s important to identify what triggers stress and to actively incorporate stress-reduction techniques into daily routines to help manage gastroparesis symptoms more effectively.
Importance of Regular Exercise
While high-intensity workouts may not always be suitable for individuals with gastroparesis, engaging in regular, gentle exercise can be beneficial. Activities such as walking, swimming, or light cycling can improve digestion and overall well-being without overexerting the body. Exercise helps by enhancing blood flow, which can aid in better digestion and can also improve mental health, reducing feelings of stress or depression that may accompany chronic conditions. Consultation with a healthcare provider is recommended to tailor an exercise plan that is appropriate and safe for your specific condition.
Support Systems and Resources
Dealing with gastroparesis can feel isolating at times, but building a strong support system can make a significant difference. Connecting with friends and family who understand your condition can provide emotional support. Additionally, joining a support group, whether in-person or online, can offer a sense of community and provide an opportunity to share experiences, tips, and encouragement with others who are facing similar challenges.
Several organizations and websites dedicated to digestive health can also serve as valuable resources for information, help in managing symptoms, and finding treatment options. Remember, you’re not alone, and there are communities and resources available to support you through your journey with gastroparesis.
Conclusion: Living with Gastroparesis
Living with gastroparesis can be challenging, but it is manageable with the right approach and support. Despite the hurdles it presents, many individuals find successful ways to manage their symptoms and lead fulfilling lives. By following a tailored treatment plan, maintaining a suitable diet, and utilizing support systems, those affected can significantly improve their quality of life. It’s crucial to work closely with healthcare professionals to monitor the condition and adjust treatments as necessary.
Remember, you are not alone, and there are resources and communities available to help navigate the complexities of living with this stomach motility disorder. Stay informed, stay hopeful, and take it one day at a time.