Breast cancer remains one of the most common cancers among women worldwide, affecting millions of lives each year. Early detection through proper screening can significantly improve the chances of successful treatment and survival. Understanding the various breast cancer screening tests and adhering to recommended guidelines is crucial.
This blog aims to enlighten women about the available screening options and the latest recommendations to help detect breast cancer in its earliest stages, potentially saving lives.
The Importance of Breast Cancer Screening
Breast cancer screening tests are vital tools designed to detect breast cancer at an early stage, even before symptoms arise. Screening aims to find cancers when they are easier to treat and more likely to respond positively to therapy, potentially leading to better outcomes. The primary goal is to uncover and treat cancers early, ideally increasing the chances of survival and reducing the need for intensive treatments. These screening tests are recommended based on factors including age, family history, and genetic predisposition, making it crucial for individuals to discuss their specific risks with healthcare providers.
Benefits of Early Detection
The most significant benefit of early detection through breast cancer screening is the potential to save lives. Studies have shown that early diagnosis of breast cancer can lead to higher survival rates, as the cancer can be treated before it spreads to other parts of the body. Additionally, early detection often allows for more treatment options, which can be less invasive and have fewer side effects. For many women, early detection also provides psychological benefits, giving a sense of control and reducing anxiety about the disease. This proactive approach emphasizes the importance of regular screenings in maintaining women’s health and well-being.
Various Breast Cancer Screening Tests:
- Mammograms
Mammograms are the most common breast cancer screening test and are considered the gold standard for early detection. A mammogram is an X-ray picture of the breast that can often find tumors that are too tiny to feel. Screening mammograms are recommended every one to two years for women over the age of 40, although those with a higher risk may need to start earlier. Mammograms can detect irregularities or masses in the breast tissue, leading to early intervention and treatment planning.
- Clinical Breast Exams
A clinical breast exam (CBE) is performed by a healthcare professional who uses their hands to examine the breasts for lumps or other changes. While CBEs are less detectable than mammograms, they can still play an essential role in detecting abnormalities, especially in populations less accessible to advanced imaging. It is usually recommended that women have a CBE at least every three years starting in their 20s and annually after the age of 40.
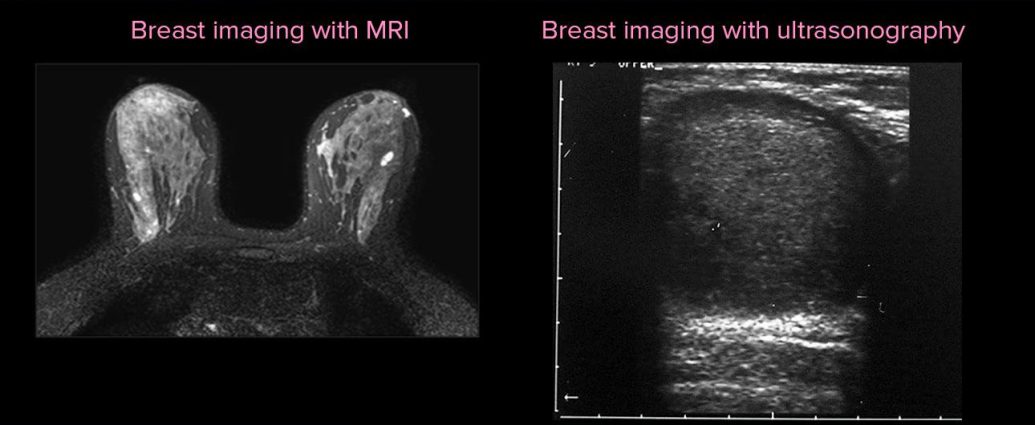
- Imaging Tests: MRI, Ultrasound
Besides mammograms, other imaging tests such as MRI (Magnetic Resonance Imaging) and ultrasound are also utilized in breast cancer screening, particularly for those at high risk or with dense breast tissue. MRIs use magnetic fields to produce detailed images of the breast, which can be more useful for younger women with denser breasts. Ultrasound is used to examine specific areas of concern found during a mammogram or CBE. This test uses sound waves to create images of tissues inside the body and is particularly good at distinguishing between solid masses, such as tumors, and cysts filled with fluid.
Guidelines for Breast Cancer Screening:
Understanding when and how often to undergo breast cancer screening is crucial for effective early detection. Different leading health organizations provide varying guidelines based on the latest research. Here, we explore the recommendations from the American Cancer Society (ACS) and the US Preventive Services Task Force (USPSTF), two authoritative sources in the realm of cancer prevention.
American Cancer Society Recommendations
The American Cancer Society advocates for women to commence annual mammograms at age 45 and continue through age 54. Women aged 55 and older may switch to biennial screening or choose to continue yearly mammograms if they wish. The initiation of screening at age 45 is based on statistical data indicating a higher probability of developing breast cancer as age progresses. ACS also allows for women aged 40 to 44 to begin annual mammograms if they desire earlier screening.
US Preventive Services Task Force Guidelines
In contrast, the US Preventive Services Task Force (USPSTF) recommends that women start biennial screenings at age 50 and continue until they are 74. The decision to start screening mammography in women before age 50 should be an individual one, taking into account patient context and values. The USPSTF highlights that the decision to undergo early screening should critically evaluate the potential benefits and harms. This recommendation places a strong emphasis on the need for personalized screening strategies rather than a broad, uniform approach.
Recommendations Based on Risk Factors:
Breast cancer screening guidelines are often adjusted depending on individual risk factors. This personalized approach aims to maximize the benefits of screening while minimizing unnecessary exams and potential anxiety for women with different levels of risk.
Family History
Women with a strong family history of breast cancer may need to start screening earlier than the general guidelines suggest. In cases where a woman’s mother, sister, or daughter has been diagnosed with breast cancer, the likelihood of developing breast cancer increases, and screening recommendations typically advise beginning up to ten years before the age at which the youngest family member was diagnosed.
Genetic Mutations
Carriers of genetic mutations such as BRCA1 or BRCA2, which significantly increase the risk for breast cancer, are advised to follow specific screening protocols. This can include starting mammograms by age 30 or even earlier, depending on the individual’s circumstances. Supplemental screenings, such as MRI scans, may also be recommended due to their increased sensitivity, especially in dense breast tissue which is typical in younger women.
Prior History of Breast Cancer
For women who have been previously diagnosed with breast cancer, guidelines recommend continual vigilance with more frequent mammograms or additional imaging tests like ultrasounds or MRIs tailored to their specific case. The recurrence risk is influenced by the type of cancer, the treatment received, and ongoing risk factors, thus requiring a customized screening approach to monitor for any signs of recurrence effectively.
Such tailored recommendations emphasize that while general guidelines provide a framework, individual circumstances significantly influence screening protocols. Thus, discussing personal and family medical history with a healthcare provider is essential for determining the most appropriate screening schedule.
Screening Frequency and Age Considerations:
Understanding when and how often to undergo breast cancer screening can significantly impact the effectiveness of early detection. Guidelines may vary between different health organizations, but they generally aim to balance the benefits of early cancer detection with the risks involved in the screening processes.
- Age to Begin Screening
The age to start breast cancer screening largely depends on individual risk factors, but there are general guidelines to help women decide when to begin. For most women, it is recommended to start getting mammograms at age 40. However, some organizations such as the American Cancer Society suggest beginning annual screening at age 45 and then transitioning to biennial screening after age 55, unless a higher risk of breast cancer is indicated. Women with a family history of breast cancer or other significant risk factors may need to start screening earlier, often ten years before the age at which their youngest family member was diagnosed with breast cancer.
- Frequency of Mammograms
Once screening begins, the frequency of mammograms should be determined based on age, personal health history, and family history. Typically, women aged 40 to 54 are advised to have mammograms annually. For women 55 and older, it’s generally acceptable to switch to mammograms every two years, provided there are no additional risk factors or previous findings that might suggest more frequent screening. This biennial approach is supported by research suggesting that it maintains nearly the same benefits in terms of cancer detection but with reduced exposure to radiation and fewer false positives.
Additional Screening Options:
While mammograms are the standard screening tool for breast cancer, additional methods are used to enhance breast cancer detection, particularly in women at high risk or with dense breast tissue.
- 3D Mammography
3D mammography, also known as digital breast tomosynthesis, is a new technology that captures multiple breast images to create a three-dimensional picture. This technology has been shown to improve the accuracy of breast cancer screening by allowing radiologists to examine breast tissue one layer at a time. 3D mammography is particularly beneficial for women with dense breasts, as it makes it easier to spot abnormalities hidden in the tissue.
- Breast MRI for High-Risk Women
For women considered to be at high risk for breast cancer (a lifetime risk of 20% or greater), an annual MRI is often recommended in addition to a mammogram. High-risk groups include those who have a known BRCA1 or BRCA2 gene mutation, have a first-degree relative with a BRCA mutation, or received radiation therapy to the chest between the ages of 10 and 30. MRI, or Magnetic Resonance Imaging, uses magnets and radio waves to produce detailed images of the inside of the breast, which can be more effective than mammograms alone in detecting cancer in dense breast tissue. However, because MRIs can lead to more false positives, they are not generally recommended for women at average risk.
Importance of Self-Exams:
Regular self-exams are a crucial component in the early detection of breast cancer. By familiarizing themselves with the normal look and feel of their breasts, individuals can more readily notice any changes, no matter how small. Changes can include lumps, thickening, or changes in the skin or nipple. Engaging in monthly self-exams can lead to early identification of potential issues, which is often key to successful treatment outcomes.
Self-exams should be performed at the same time each month. For women who are menstruating, it is recommended to conduct the exam several days after the menstrual cycle ends, as this is when breasts are least likely to be swollen or tender. Here are some steps to follow during a self-exam:
– Begin by looking at your breasts in the mirror with your shoulders straight and your arms on your hips. Look for any changes in size, shape, or symmetry, as well as any visible distortions or swelling.
– Raise your arms and look for the same changes.
– While lying down, use your right hand to feel your left breast and then your left hand to feel your right breast, using a firm, smooth touch with the first few finger pads of your hand. Follow a pattern to ensure all the breast tissue is covered.
– Finally, feel your breasts while you are standing or sitting, using the same hand movements.
Understanding how to properly conduct a breast self-exam and what to look for can empower individuals in their health management, potentially leading to earlier detection of abnormalities.
Conclusion: Importance of Regular Screening and Early Detection in Breast Cancer
The pursuit of regular breast cancer screening is a critical measure in maintaining women’s health. Early detection not only enhances the possibility of successful treatment but significantly lowers the risk of severe interventions. Studies consistently underscore that cancers detected at an early stage are generally easier to treat effectively, often resulting in better outcomes and reduced treatments.
Regular screenings facilitate the monitoring of changes in breast tissue over time, providing a crucial advantage in identifying abnormalities as early as possible. Moreover, through adherence to recommended screening guidelines, individuals are empowered to make informed decisions, fostering a proactive approach to their health.
Thus, embracing a schedule of regular breast cancer screenings is a profound step towards safeguarding one’s well-being, ensuring peace of mind, and championing health longevity.