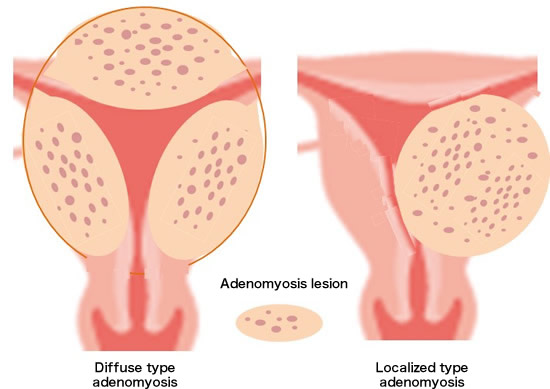
Adenomyosis is a relatively obscure yet significantly impactful condition affecting women, primarily nestled within the domain of uterine health. It is characterized by the unwelcome intrusion of endometrial tissue—the lining that usually covers the inside of the uterus—into the muscular wall of the uterus, known as the myometrium. This invasion can lead to a spectrum of symptoms, ranging from mildly uncomfortable to severely debilitating, profoundly affecting the quality of life of those it touches.
For many women, the journey toward understanding and managing adenomyosis begins with recognizing its signs and symptoms. These commonly include heavy menstrual bleeding, severe menstrual cramps that may worsen over time, pain during intercourse, and chronic pelvic pain. The condition is somewhat of an enigma, as it shares symptoms with other gynecological conditions, making its diagnosis a process of exclusion and careful medical evaluation.
The purpose of this discussion is not merely to decipher the complexities of adenomyosis but to illuminate the pathways to managing and living with this condition. We will explore its symptoms, delve into the reasons behind its occurrence, evaluate diagnostic methods, and review current treatments available. Through this exploration, we aim to empower women with knowledge, facilitating a proactive approach to their uterine health and overall well-being.
Causes of Adenomyosis:
The precise origins of adenomyosis, a condition where the inner lining of the uterus breaks through the muscle wall of the uterus, remain somewhat shrouded in mystery. Medical professionals and experts have, however, identified several potential contributing factors that might explain why some women develop this painful condition.
- Hormonal Imbalance
A recurring theme in discussions about adenomyosis is the role of hormonal imbalance. Estrogen, in particular, seems to play a critical part. This hormone, which regulates the menstrual cycle and prepares the uterus for pregnancy, is believed to stimulate the growth of adenomyosis. Fluctuations in hormone levels, especially during perimenopause, can intensify the condition. Progesterone, another hormone related to the menstrual cycle and pregnancy, also interacts with estrogen in ways that might exacerbate adenomyosis. Furthermore, other hormones like prolactin and follicle-stimulating hormone (FSH) could potentially have a role in the development of this condition, although their exact contributions are less clear.
- Invasive Uterine Procedures
Another recognized risk factor for adenomyosis is the history of invasive uterine procedures. This includes surgeries such as cesarean sections (C-sections), fibroid removal surgeries (myomectomies), and procedures to remove uterine polyps or to diagnose and treat other uterine conditions (hysteroscopies). These interventions might inadvertently encourage the invasion of the endometrial cells into the myometrium (the muscular wall of the uterus), essentially providing a pathway for adenomyosis to develop. Trauma to the uterine lining, whether from childbirth or surgical interventions, can therefore be a significant precursor to adenomyosis.
Symptoms of Adenomyosis:
Identifying adenomyosis can be challenging, as its symptoms are commonly shared with other gynecological conditions. Yet, two hallmark symptoms distinctly associated with adenomyosis are severe pelvic pain and heavy menstrual bleeding. Understanding these symptoms is crucial for individuals seeking diagnosis and treatment.
- Severe Pelvic Pain
For many, the pain associated with adenomyosis is more than just discomfort; it’s a severe and debilitating cramp that can affect their quality of life. This pain is not limited to the menstrual period; it can persist throughout the menstrual cycle, with some sufferers experiencing chronic pelvic pain. The intensity of the pain might be linked to the extent of the adenomyosis, with those having a more extensive invasion into the uterine muscle experiencing worse symptoms. Additionally, pain during intercourse is a significant concern for those with adenomyosis, further impacting their personal lives and relationships.
- Heavy Menstrual Bleeding
Another significant symptom of adenomyosis is heavy menstrual bleeding, also known as menorrhagia. Those affected may experience prolonged periods lasting more than seven days and have to change their sanitary products far more frequently than usual, including during the night. This symptom can contribute to anemia, leading to fatigue and further exacerbating the feeling of being unwell. It’s not uncommon for clots to be present in the menstrual blood, and for some, the bleeding can be so severe that it disrupts daily activities, necessitating medical intervention to manage the symptoms.
In both these symptoms, the severity and impact on an individual’s life can vary widely. Some may find their symptoms manageable with minimal intervention, while others might require comprehensive treatment strategies to find relief. Understanding the full scope of adenomyosis symptoms is essential for navigating this often painful condition.
Diagnosis of Adenomyosis:
Understanding the presence of adenomyosis, a condition characterized by the growth of endometrial tissue within the muscular wall of the uterus, necessitates detailed diagnostic procedures. These are essential for confirming the condition and facilitating effective treatment plans tailored to the needs of each woman experiencing its often debilitating symptoms. Diagnosis primarily relies on imaging studies, which are critical in distinguishing adenomyosis from other similar gynecological conditions.
- Ultrasound Imaging
Ultrasound imaging stands at the forefront of diagnosing adenomyosis. This non-invasive technique, employing sound waves to create images of the uterine structure, allows healthcare providers to identify characteristic signs of adenomyosis. These may include a thickening of the uterine walls or the presence of cysts within the muscle layer. Transvaginal ultrasound, where the device is inserted into the vagina, offers more detailed images of the uterus compared to the abdominal ultrasound. However, the interpretation of these images requires a considerable degree of expertise, as the visual cues of adenomyosis can sometimes be subtle or mimic those of other uterine conditions.
- Magnetic Resonance Imaging (MRI)
For cases where ultrasound results are inconclusive, or when a precise mapping of adenomyosis is necessary for treatment planning, Magnetic Resonance Imaging (MRI) is the next step. MRI uses powerful magnetic fields and radio waves to generate comprehensive images of the organs within the pelvis. Its high-resolution images allow for an accurate assessment of the extent and distribution of adenomyosis within the uterus. Unlike ultrasound, MRI is more definitive in distinguishing adenomyosis from uterine fibroids, another common gynecological issue, thereby ensuring an accurate diagnosis.
Treatment Options for Adenomyosis:
Once a diagnosis of adenomyosis is confirmed, a multidimensional treatment approach is usually recommended to manage symptoms and improve quality of life. While treatment may vary based on the severity of symptoms, the desire for future pregnancies, and other individual considerations, it generally includes pain management, hormonal therapies, and, in some cases, surgical interventions.
Pain Management Medications:
The cornerstone of adenomyosis symptom management is often pain relief. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen are commonly prescribed to reduce pelvic pain and decrease heavy menstrual bleeding. These should be taken before or at the onset of menstruation to be most effective. For more severe pain, physicians may recommend stronger prescription pain relievers. These medications, however, are not without their side effects and should be used under careful medical supervision.
Hormonal Therapies
Hormonal therapies aim to control or halt the growth of adenomyosis tissue, thereby alleviating symptoms. Various hormonal treatments can be effective, including:
- Birth control pills: Help regulate menstrual cycles and reduce heavy bleeding.
- Progestin therapy: Delivered via pills, an intrauterine device (IUD), or injections, progestin can decrease pain and bleeding.
- Gonadotropin-releasing hormone (GnRH) agonists: These medications temporarily induce a “menopausal” state, shrinking adenomyosis lesions by reducing estrogen levels. However, their use is generally limited in duration due to potential side effects.
Minimally Invasive Surgical Procedures
For women who do not respond to medication or are seeking a more definitive solution, minimally invasive surgical procedures may be considered. These can include:
- Uterine artery embolization: Targets and blocks the blood supply to the adenomyosis lesions, causing them to shrink.
- Endometrial ablation: Destroys the lining of the uterus to reduce menstrual bleeding, though not advised for women wishing to conceive.
- Myometrial excision: Removes the adenomyotic tissue while preserving the uterus. This option, however, is complex and requires a specialist with expertise in such surgery.
Each surgical option carries risks and potential impacts on fertility, underscoring the importance of a thorough discussion with a healthcare provider to determine the most suitable course of action.
Lifestyle Changes for Managing Adenomyosis:
Adenomyosis is a challenging condition, that impacts the quality of life for many women. It can prompt symptoms like heavy periods and severe pelvic pain. Alongside medical treatments, several lifestyle adjustments can significantly improve symptom management. Embracing these changes not only helps in alleviating physical discomfort but also enhances overall well-being.
- Dietary Adjustments
Diet plays a crucial role in managing adenomyosis symptoms. Incorporating foods rich in omega-3 fatty acids, such as salmon and flaxseeds, can help reduce inflammation. Additionally, consuming plenty of fruits, vegetables, and whole grains ensures a high intake of vitamins and minerals, supporting general health and possibly reducing pelvic pain. On the other hand, it’s advisable to limit the intake of red meat, processed foods, and sugar to prevent exacerbating inflammation.
- Regular Exercise
Regular physical activity is beneficial for women with adenomyosis. Exercise can help in reducing pain by increasing blood flow and reducing stress. Engaging in low-impact activities, such as walking, swimming, or yoga, can be particularly effective. Not only does it help with symptom management, but it also boosts mental health, providing a sense of well-being.
- Stress Management Techniques
Stress exacerbates the symptoms of many health conditions, including adenomyosis. Implementing stress management techniques such as deep breathing exercises, meditation, or mindfulness can be remarkably effective. These practices not only help in managing stress but also promote relaxation, which can lead to a decrease in pelvic pain intensity.
- Support Networks
Coping with the symptoms of adenomyosis can be emotionally taxing. Building a support network of friends, and family, or joining support groups for women with uterine health issues can provide emotional relief. Sharing experiences and tips can foster a sense of community and lessen the burden of the condition.
By incorporating these lifestyle changes, women with adenomyosis can experience significant improvements in their symptoms. While these adjustments may not cure the condition, they can greatly enhance the quality of life and overall health.
Conclusion: Empowering Women Through Knowledge of Adenomyosis
Understanding the complex realm of adenomyosis is a fundamental step in empowering women to make informed decisions about their health. Knowledge about this condition not only demystifies the symptoms of severe pelvic pain and heavy periods but also opens the doorway to seeking suitable treatment and support. Women need to recognize that they are not alone in this journey and that their symptoms are valid and deserving of attention.
By keeping informed about adenomyosis, women can actively participate in their healthcare decisions, advocate for their needs, and explore the most effective treatment options available. Discussions with healthcare providers become more meaningful when armed with knowledge, leading to personalized care plans that consider the physical, emotional, and lifestyle impacts of adenomyosis.
In wrapping up, it’s clear that the path to understanding and managing adenomyosis is multifaceted, requiring a coalition of medical guidance, personal research, and community support. Remember, prioritizing uterine health is a crucial aspect of women’s health, and every woman deserves to lead a life free from the debilitating effects of adenomyosis. Knowledge is power, and in the case of adenomyosis, it’s a critical step toward regaining control over one’s health and well-being.