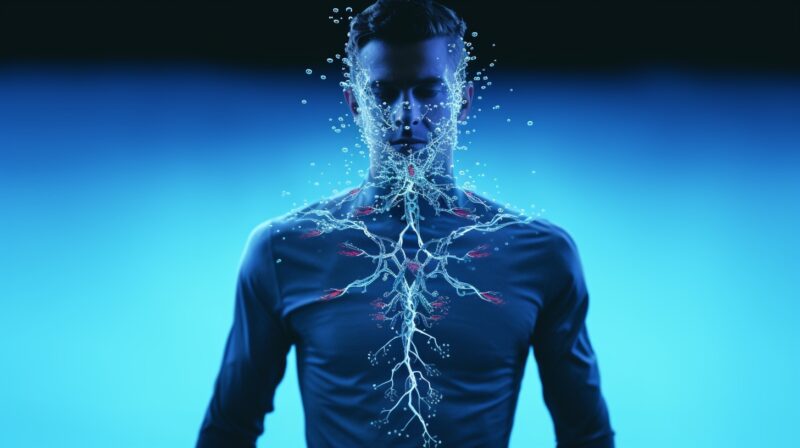
Dealing with exposure to infected bodily fluids can be a daunting experience, yet it’s a reality faced by healthcare professionals, first responders, and sometimes, even the general public. Whether it’s through an unforeseen accident, caregiving, or in a professional setting, knowing the right steps to take immediately after such exposure is crucial for your safety and well-being.
Infected bodily fluids, including blood, saliva, semen, vaginal secretions, and any other fluid containing visible blood, have the potential to transmit infections if not handled properly. This guide aims to equip you with the necessary knowledge and procedures to manage these situations effectively, minimizing the risk of infection and ensuring that the proper safety measures are followed.
Understanding the Risks of Exposure to Infected Bodily Fluids:
Exposure to infected bodily fluids can pose significant health risks. These bodily fluids include blood, urine, feces, saliva, vomit, and other secretions that may carry infectious pathogens such as viruses, bacteria, or fungi. Understanding the types of fluids and the risks associated with exposure is crucial for ensuring personal safety and taking appropriate measures to prevent transmission of infections.
Types of Infected Bodily Fluids:
Infected bodily fluids are those that carry pathogens capable of causing diseases. Common types of these fluids include:
- Blood: Carries a high risk of transmitting bloodborne diseases like HIV, hepatitis B, and hepatitis C.
- Saliva: Can transmit diseases such as mononucleosis, also known as the “kissing disease,” and certain types of coronavirus, including the virus that causes COVID-19.
- Urine and Feces: These can carry pathogens responsible for diseases like E. coli infections, hepatitis A, and parasitic infections.
- Vomit: May contain infectious agents, especially if the underlying cause of vomiting is an infectious disease.
- Semen and Vaginal Secretions: Can transmit sexually transmitted infections (STIs) such as HIV, herpes, syphilis, and gonorrhea.
- Breast Milk: Known to potentially transmit HIV and cytomegalovirus (CMV) to infants.
Understanding the types of fluids and their associated risks is essential in healthcare settings, laboratories, and everyday situations where exposure might occur.
Risks Associated with Exposure:
The risks of exposure to infected bodily fluids vary depending on the type of fluid, the pathogen involved, and the mode of exposure. Commonly transmitted diseases through bodily fluids include:
- Bloodborne diseases: These are among the most serious and include HIV, hepatitis B, and hepatitis C, which can have long-lasting health impacts.
- Gastrointestinal infections: Caused by exposure to feces or vomit, these include illnesses like norovirus, E. coli, and salmonella.
- Respiratory infections: Saliva droplets can transmit diseases like influenza, COVID-19, and the common cold.
- STIs: Exposure to semen and vaginal secretions can result in the transmission of diseases such as HIV, chlamydia, and syphilis.
Understanding these risks is crucial for implementing effective prevention and response strategies.
Safety Measures to Prevent Exposure:
To prevent the transmission of infections through infected bodily fluids, adopting appropriate safety measures is crucial, especially in environments where exposure risk is higher. This involves using proper protective gear and following precautionary steps meticulously.
Proper Protective Gear to Use:
When handling or potentially being exposed to infected bodily fluids, wearing the right protective gear can significantly reduce the risk of transmission. Essential items include:
- Gloves: Wear disposable gloves when you might come into contact with bodily fluids. Ensure they are the right size and replace them after each use.
- Gowns or Aprons: These provide an extra layer of protection, especially during tasks prone to splashes or extensive contact with bodily fluids.
- Masks and Face Shields: Masks protect you from inhaling infectious agents, while face shields protect the eyes and face from splashes.
- Shoe Covers: In environments where floor contamination might occur, shoe covers can prevent the spread of infectious agents.
It is also important to understand the proper way to don and doff this protective gear to prevent self-contamination.
Precautionary Steps to Take in High-Risk Environments:
In addition to wearing proper protective gear, certain behaviors and practices can help minimize the risk of exposure:
- Hand Hygiene: Frequently wash hands with soap and water for at least 20 seconds, especially after removing gloves or other protective gear.
- Safe Handling Practices: Use tools like tongs, forceps, or disposable paper to handle items contaminated with bodily fluids. Avoid splashing or aerosolizing the fluids.
- Disposal: Discard any materials contaminated with bodily fluids in designated biohazard containers. Ensure these materials are handled according to local regulations for biomedical waste.
- Education and Training: Regular training on the proper use of protective gear and safe handling practices is crucial, especially for professionals working in health care or laboratory settings.
By understanding the risks associated with exposure to infected bodily fluids and strictly adhering to safety measures, individuals can significantly reduce the risk of infection and ensure a safer environment for everyone involved.
Immediate Steps to Take After Exposure:
When you realize you’ve come into contact with infected bodily fluids, the situation can be alarming. However, it’s crucial to act promptly and efficiently to mitigate risks. The initial moments after exposure are pivotal in preventing infection.
Washing the Affected Area Thoroughly
The first and most immediate step to take is to thoroughly wash the affected area. If the skin is the contact point, use soap and warm water to clean the area gently but thoroughly for at least 20 seconds. In case infected bodily fluids come into contact with your mucous membranes (e.g., eyes, mouth), flush the area with copious amounts of water or saline solution. This immediate action can greatly reduce the risk of infections, as it helps remove a significant portion of the potentially infectious materials. Avoid scrubbing the area harshly, as this may cause abrasions that could further facilitate the entry of pathogens.
Seeking Medical Help Promptly
After washing the affected area, it is essential to seek medical help as soon as possible. Inform the healthcare provider about the exposure incident, including the type of fluid you were exposed to, the source of the infection (if known), and the method and duration of exposure. Healthcare professionals can assess the situation and provide post-exposure prophylaxis (PEP) if necessary. This may include vaccinations, medications, or specific treatments to prevent infection. Early medical intervention is key to minimizing the risk of contracting diseases from infected bodily fluids.
First Aid Practices for Different Types of Exposure to Infected Bodily Fluids:
Understanding the appropriate first aid measures for different types of exposure to infected bodily fluids is crucial. Whether it’s skin, eye, or inhalation exposure, knowing the correct protocols can significantly aid in preventing infections.
Skin Exposure
If infected bodily fluids come into contact with the skin, especially if there are cuts, abrasions, or any other forms of broken skin, immediate and thorough cleaning is crucial.
- Immediately wash the area with soap and water.
- If available, an antiseptic solution may be applied after washing to further reduce the risk of infection.
- Cover any exposed wounds with a sterile dressing after cleaning to prevent secondary infections.
- Even if the skin seems intact, it’s advisable to clean the area thoroughly as a precautionary measure.
Eye Exposure
Eyes are particularly sensitive, and exposure requires careful attention.
- Rinse your eye(s) immediately and continuously with lukewarm water or an isotonic saline solution for at least 15 minutes. It is important to keep the eyelids open to ensure that all parts of the eye are thoroughly washed.
- Do not rub the eyes, as this may cause further irritation or damage.
- After flushing, seek medical evaluation, especially if irritation, pain, or visual disturbances persist.
Ingestion or Inhalation Exposure:
Although less common, ingestion or inhalation of infected bodily fluids poses a significant health risk that requires specific first-aid measures.
- In case of ingestion, do not induce vomiting. Rinse your mouth thoroughly with water and spit it out. Avoid swallowing any potentially contaminated fluids.
- If you suspect inhalation exposure, move immediately to an area with fresh air. Monitor for any difficulty in breathing, coughing, or wheezing.
- For both ingestion and inhalation exposure, seek medical attention promptly. Provide detailed information about the incident to the healthcare provider for accurate assessment and appropriate intervention.
In all cases, it’s essential to follow up with appropriate medical evaluation and treatment. Post-exposure prophylaxis (PEP), when started early, can be instrumental in preventing infection following exposure to infected bodily fluids. Awareness and immediate action are key components in handling such exposures safely and effectively.
Importance of Seeking Professional Help After Exposure:
Seeking professional medical help immediately after being exposed to infected bodily fluids is crucial for your health and safety. Medical professionals can provide accurate assessments and necessary treatments to prevent infections or diseases from developing or worsening. Ignoring potential exposure can lead to severe health complications, underscoring the urgency of seeking expert advice and intervention.
Testing for Potential Infections
Upon consulting a healthcare provider, one of the first steps will be to conduct tests to determine if you have been infected. These tests may include, but are not limited to:
- Blood tests to check for viruses such as HIV, hepatitis B, and hepatitis C
- Tests for bacterial infections that could be present in the bodily fluid you were exposed to
Early testing allows for quicker implementation of any required treatments or preventive measures, significantly reducing the risk of future health issues. It’s essential to be transparent with your healthcare provider about the nature of your exposure to ensure you receive the most appropriate tests.
Follow-up Care and Monitoring
After initial assessments and tests, follow-up care and monitoring become key components of managing potential infections. This may involve:
- Additional testing after a certain period since some infections have incubation periods before they can be detected in tests
- Vaccinations or preventative medications in cases where exposure to certain infections has been confirmed or is highly likely
- Regular check-ups to monitor for any signs or symptoms that may develop
It’s crucial to adhere to the recommended follow-up schedule provided by your healthcare provider to ensure proper management of your health post-exposure. Ignoring follow-up care can lead to delayed diagnosis and treatment of infections, complicating your health further.